A Clinician's Guide to Bicon Dental Implants
When clinicians first encounter Bicon dental implants, it becomes clear they operate on a distinct set of bioengineering principles. This system was not designed by modifying existing screw-based mechanics; it was developed from the ground up to achieve a specific biological response. The entire concept revolves around a locking taper connection and a unique plateaued implant body, a combination that delivers exceptional stability and promotes healthy bone formation, especially in clinical scenarios with limited vertical bone height.
This guide provides a technical overview for dental professionals, students, and distributors on the core philosophy, scientific principles, and clinical workflow of the Bicon system.
Understanding the Bicon Dental Implant Philosophy

Consider common challenges in implant dentistry: screw loosening, microbial leakage at the microgap, and the frequent need for extensive bone grafting. The Bicon system was engineered specifically to address these issues. Its philosophy is to create a harmonious relationship between the implant and the surrounding bone, allowing the implant's design to encourage a positive biological response.
This approach positions Bicon as a unique solution for clinicians seeking predictable outcomes without routine reliance on invasive augmentation procedures. The system is built on two core concepts that are essential to understanding its clinical advantages.
Core Design Differentiators
The two features that truly set Bicon dental implants apart are their connection mechanism and the geometry of the implant body. Understanding these principles is key to appreciating how the system functions.
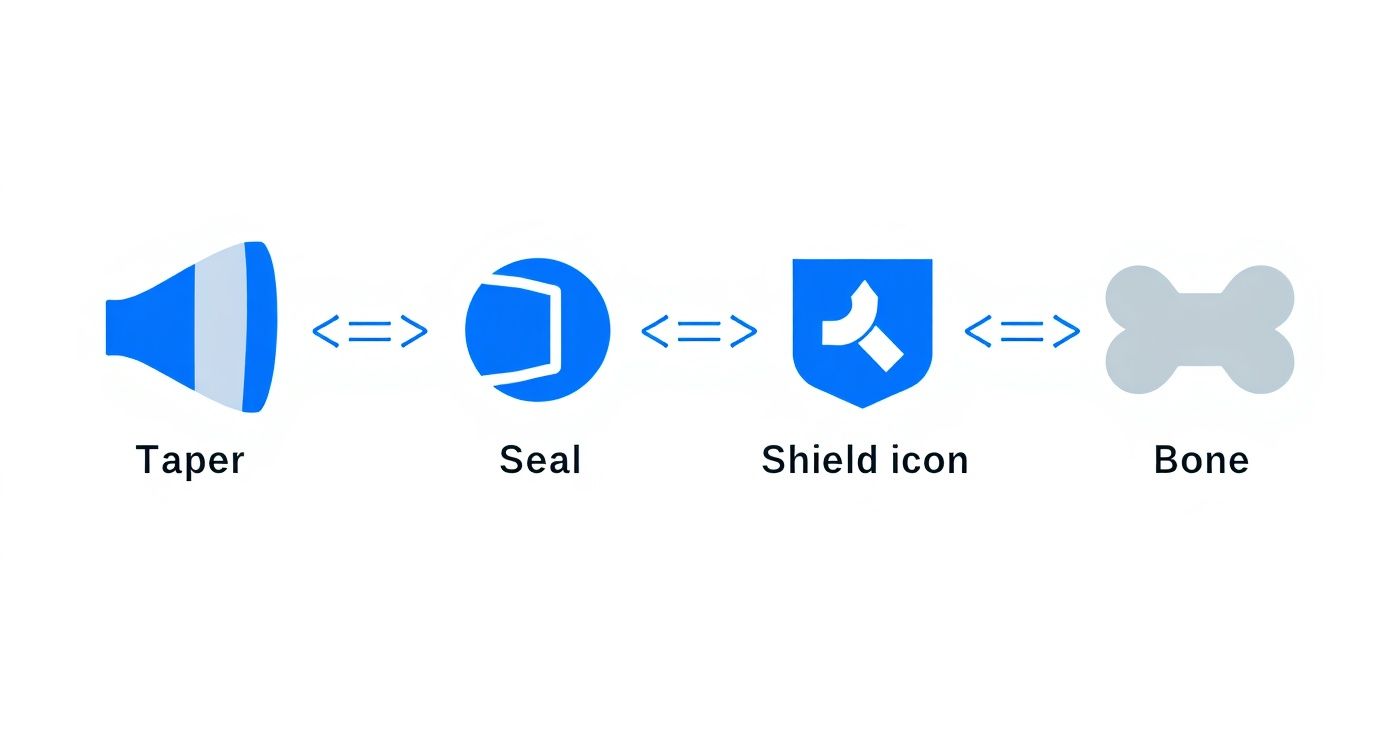
- The 1.5° Locking Taper Connection: This is a screwless, friction-fit connection that creates a hermetic seal between the implant and the abutment. Functioning like a Morse taper, it forms a "cold weld" that effectively seals the microbial microgap often associated with screw-retained designs.
- The Plateau Design: Instead of threads, the implant body features a series of flat-topped fins, or plateaus. This geometry significantly increases the implant's surface area and provides a scaffold for mature, cortical-like bone to grow vertically between the fins.
This combination provides the system with its robust stability, which is especially critical for their Bicon SHORT® Implants used in areas with minimal bone height. The demand for specialized solutions like this is growing. For instance, the German dental implants market was valued at approximately USD 429.2 million in 2024 and is projected to reach nearly USD 639.8 million by 2030. You can discover more insights about the German dental implant market trends here.
Bicon System Core Features at a Glance
The table below summarizes the primary characteristics that differentiate the Bicon system from more conventional implant designs.
| Feature | Description | Primary Clinical Advantage |
|---|---|---|
| Locking Taper Connection | A 1.5° friction-fit, screwless connection between implant and abutment. | Creates a bacterial seal, eliminating the microgap and preventing screw loosening. |
| Plateau Design | Fins instead of threads on the implant body. | Increases surface area and promotes haversian bone growth for enhanced stability. |
| Short Implant Options | Implants as short as 4.0 mm. | Allows for treatment in atrophic ridges, often avoiding the need for grafting. |
| Sloping Shoulder | The implant shoulder is angled to preserve crestal bone. | Promotes better aesthetics by maintaining the gingival architecture around the implant. |
These features work synergistically to support the system's core philosophy.
By prioritizing a bacterial seal and a bone-friendly surface, the Bicon philosophy aims to simplify complex cases, reduce the need for augmentation, and deliver durable, long-term restorative results.
Bicon provides clinicians a potent alternative for treating atrophic ridges and navigating around vital structures without compromising stability or aesthetics. For professionals interested in exploring a broad range of implant designs, including those with advanced surfaces, a review of the versatile Alfa Gate implant portfolio can offer valuable comparative insights.
The Science Behind Bicon’s Locking Taper and Plateau Design
At the heart of the Bicon dental implant system lie two design principles that fundamentally distinguish it from conventional screw-retained implants. These features represent a rethinking of the implant-abutment connection and the process of osseointegration. A technical understanding of the locking taper and plateau design is necessary to grasp the system's clinical performance.
Creating a Cold Weld with a Locking Taper
The most defining feature is the 1.5° locking taper connection. Based on the time-tested Morse taper engineering concept, this design creates a secure, friction-fit seal between the implant and the abutment.
When the abutment is seated with controlled force, the precise 1.5° angle of the two mating surfaces generates immense frictional force, locking the components together in what is often termed a “cold weld.” This mechanical fusion is strong enough to resist rotational forces without a screw.
The primary clinical benefit is the virtual elimination of the microgap at the implant-abutment connection. In typical screw-retained systems, this space can harbor bacteria, leading to inflammation and potential crestal bone loss.
By forming a hermetic seal, the Bicon locking taper shields the crestal bone from the oral environment. This is a critical factor for maintaining long-term tissue health and stable bone levels at the implant shoulder.
This design directly addresses the common issue of micromotion at the connection point, a topic further detailed in our article on the parameters determining micromotion at the implant-abutment interface. The stability of this connection is foundational to the restorative outcome.
Engineering Bone Growth with a Plateau Design
The second pillar of the Bicon philosophy is the implant body's geometry. Instead of threads, it features a series of fin-like plateaus, engineered to influence the quality of osseointegration. While threaded implants rely on mechanical interlocking, Bicon's plateaus are designed for a different biological response.
The spaces between these plateaus create a protected environment where bone can mature under physiological loading. The design promotes the formation of Haversian bone—a slower-growing, highly organized, and well-vascularized bone type that resembles native cortical bone.
- Increased Surface Area: The fins dramatically increase the functional surface area for bone-to-implant contact compared to a threaded implant of the same dimensions.
- Optimal Force Distribution: The flat tops of the plateaus distribute occlusal forces perpendicular to the bone, a stimulus that encourages bone apposition rather than resorption.
This biological response is what enables Bicon SHORT® Implants to achieve high stability, even in limited vertical bone. Since its introduction around 1985, Bicon has maintained this locking taper and plateau geometry, an approach supported by extensive clinical documentation.
Together, the locking taper and plateau design create a powerful synergy. The stable, sealed connection protects the underlying bone, while the implant body actively encourages the growth of strong, mature bone, offering clinicians a reliable tool for predictable outcomes.
Mastering the Bicon Surgical and Restorative Workflow
The Bicon workflow represents a departure from the torque-driven protocols of traditional threaded systems. It is a process that prioritizes biology over mechanical force, requiring a procedural adjustment for both surgery and restoration. Mastering this workflow can lead to highly predictable and aesthetic clinical results.
The surgical protocol is centered on slow-speed, low-heat osteotomy preparation. Bicon’s reamers operate at a gentle 50 RPM without irrigation, a technique designed to minimize thermal trauma to the bone. This method also allows for the harvesting of autogenous bone during preparation, which can be used for localized grafting.
Following osteotomy preparation, the implant is placed with a press-fit technique, gently tapped into its final position. This method seats the plateau design securely and prepares the locking taper for its connection with the abutment. This is distinct from the high-torque insertion of threaded implants and relies on a precisely prepared osteotomy for primary stability.
Restorative Simplicity with the IAC
The restorative phase highlights the efficiency of the Bicon system, particularly with its signature Integrated Abutment Crown™ (IAC). This is a one-piece, cementless, and screwless restoration where the abutment and crown are combined. By utilizing the locking taper connection, it eliminates two major complications in implant dentistry: screw loosening and the risks of residual subgingival cement.
The clinical advantages of the IAC include:
- Safe Subgingival Margins: Clinicians can confidently place restoration margins subgingivally to achieve optimal aesthetics without the risk of cement-induced peri-implantitis.
- Simplified Impressions: Impressions are taken at the abutment level, simplifying the process and enhancing accuracy.
- 360° Positional Freedom: The abutment can be rotated 360°, providing limitless positioning options and simplifying the correction of angulation issues without requiring specialized angled abutments.
The IAC can be fabricated in a laboratory or chairside, offering flexibility in the clinical workflow. This streamlined approach improves efficiency from impression to final seating. For a broader overview of surgical protocols, our dental implant surgery guide for dentists provides additional context.
Where Bicon SHORT Implants Really Shine

The unique design of Bicon dental implants makes them an effective solution for clinical scenarios that are challenging for traditional threaded systems. Their most significant advantage lies in addressing vertical bone deficiencies. In these cases, Bicon SHORT® Implants often allow clinicians to avoid complex and invasive grafting procedures.
The large surface area provided by the plateau design and the stability of the locking taper make these short implants a predictable choice for the atrophic posterior mandible or maxilla. They enable implant placement without encroaching on vital structures like the inferior alveolar nerve or the maxillary sinus. This approach challenges the traditional belief that implant length is the primary determinant of success, shifting the focus to functional surface area and biomechanics.
Avoiding Advanced Grafting Procedures
A primary indication for Bicon SHORT® Implants is the avoidance of vertical bone augmentation. Procedures such as sinus lifts and block grafts, while effective, add surgical complexity, patient morbidity, and cost.
For the patient, selecting a short implant translates to a less invasive surgery, a more comfortable recovery, and a shorter time to final restoration. For the clinician, it means mitigating risks associated with grafting, such as membrane perforation or graft failure, and simplifying treatment planning.
By placing a 5.0 mm or 6.0 mm implant directly into native bone, clinicians can often bypass augmentation entirely, delivering a fixed restoration without the biological and financial burden of major grafting surgery.
This makes Bicon dental implants an excellent option for patients who are not ideal candidates for extensive surgery or who prefer a simpler, more cost-effective solution.
Restoring in Anatomically Constrained Sites
Bicon also excels in anatomically constricted spaces. Its narrow implant options are well-suited for challenging areas like missing maxillary lateral incisors or single mandibular incisors, where bone and soft tissue volume are critical for an aesthetic outcome.
The implant's sloping shoulder design is key in these situations. This feature helps preserve crestal bone height and provides space for the interdental papillae, contributing to a natural gingival emergence profile.
- Maxillary Lateral Incisors: These sites are known for limited mesiodistal space. A narrow-diameter implant that minimizes surgical trauma is ideal.
- Mandibular Incisors: The thin labial bone and tight spacing in the lower anterior region demand precision. An implant designed to work with the local biology is essential.
In both scenarios, the objective is a stable, functional, and aesthetic restoration. When bone regeneration is unavoidable, staying informed on current techniques is crucial. You can explore this topic further in our article on modern bone regeneration strategies. Smart case selection, based on a thorough clinical and radiographic evaluation, remains the foundation of successful implant dentistry.
Getting to Grips with Bicon Prosthetics and Lab Communication
Successful restoration of Bicon implants depends on two factors: a thorough understanding of the unique prosthetic components and clear communication with the dental laboratory. The workflow is built around the locking taper connection, which offers distinct restorative advantages but requires a specific approach from both the clinician and the technician.
The centerpiece of the restorative system is the Integrated Abutment Crown™ (IAC), a single unit combining the abutment and crown. This design addresses two significant challenges in implant dentistry: the biological risk of subgingival cement and the mechanical risk of screw loosening. The IAC allows for confident subgingival margin placement for superior aesthetics without the associated complications.
Mastering Abutment Selection
The first critical restorative decision is selecting the correct abutment. Bicon offers a range of options, from temporary healing abutments designed to sculpt the gingiva to the final restorative abutments that support the IAC.
A key feature is the universal abutment design, which offers a full 360° of rotational freedom. This provides exceptional flexibility for correcting angulation and achieving the ideal occlusion directly at the chair. This simplifies the restorative process significantly, as a single universal abutment can often be prepared to fit the case, reducing the need to stock numerous angled abutments.
Bicon Prosthetic Abutment Selection Guide
This table outlines the common Bicon abutment types and their clinical applications to assist in proper selection.
| Abutment Type | Primary Use Case | Material | Key Clinical Note |
|---|---|---|---|
| Healing Abutment | Gingival tissue forming and protection during osseointegration. | Titanium Alloy, PEEK | Select size based on desired emergence profile and inter-arch space. |
| Temporary Abutment | Fabricating provisional restorations for immediate function or aesthetics. | PEEK, Resin | Essential for maintaining soft tissue architecture before the final crown. |
| Impression Post | Transferring the implant position accurately to the master cast. | Stainless Steel | Snaps securely into the implant well for a precise, stable impression. |
| Restorative Abutment | Foundation for the final Integrated Abutment Crown (IAC). | Titanium Alloy | Offers 360° positioning for unlimited corrective possibilities. |
Nailing Your Laboratory Communication
Clear communication with your dental laboratory is non-negotiable, especially if the lab is unfamiliar with the Bicon system. A detailed prescription is essential to prevent errors and ensure the final restoration meets clinical expectations.
Your lab prescription should include:
- Implant Details: Specify the exact diameter and length of the placed Bicon implant.
- Abutment Information: Clearly state the type and size of the restorative abutment used.
- Desired Restoration: Explicitly request an Integrated Abutment Crown (IAC) and specify the material (e.g., porcelain-fused-to-metal, all-ceramic).
- Shade and Occlusal Scheme: Include all standard restorative details.
Pro Tip: Proactively communicate with your laboratory technician before sending the case. A brief discussion to confirm their familiarity with the Bicon locking taper and the IAC fabrication process can prevent significant delays and remakes.
With a solid grasp of abutment selection and disciplined lab communication, delivering durable and aesthetic restorations with the Bicon system becomes a predictable and efficient process.
Troubleshooting Common Clinical Challenges
Every implant system presents unique clinical situations. Proficiency with Bicon dental implants involves understanding how to manage scenarios that differ from threaded implant protocols. Anticipating potential issues and having a clear management plan is key to clinical success.
A common question relates to achieving primary stability. Since placement is a press-fit technique, the tactile feedback differs from torque-driven insertion. If an implant feels loose upon seating, it typically indicates an over-prepared osteotomy. The solution is to remove the implant and prepare the site for the next larger implant diameter, ensuring a snug and secure fit.
Retrieving Seated Abutments
Another unique challenge is the retrieval of a fully seated abutment. The locking taper creates a strong connection, which is excellent for prosthetic stability but requires a specific technique for removal.
Specialized abutment removal forceps are used for this purpose. The abutment is gripped firmly, and a gentle, controlled rotational or rocking motion is applied to break the frictional lock.
The key is to use gradual, steady force rather than a sudden jerk. This disengages the taper safely and predictably without transferring excessive force to the implant-bone interface.
Optimising Soft Tissue Management
Achieving an aesthetic outcome with Bicon dental implants is highly dependent on effective soft tissue management. The system’s sloping shoulder is designed to preserve crestal bone and support healthy papillae, but the clinician must guide the emergence profile.
Using the correctly sized healing abutment is critical for sculpting the gingiva during the healing phase. This prepares the soft tissue architecture for the final Integrated Abutment Crown (IAC), ensuring a natural transition from the restoration to the surrounding gums.
For complex cases like overdentures or full-arch restorations, meticulous planning is paramount. The system's abutment flexibility simplifies these treatments, but achieving a passive prosthetic fit requires precise impressions and clear lab communication. For clinicians new to these advanced applications, mentorship or additional training is highly recommended.
By understanding these common clinical scenarios and their solutions, practitioners can progress from basic proficiency to mastery of the system.
Answering Your Top Questions About Bicon Implants
When evaluating a new implant system, practical questions about its clinical application are most important. Here are answers to some of the most common queries from dental professionals regarding Bicon dental implants.
How Does the Locking Taper Prevent Screw Loosening?
The Bicon system eliminates screws entirely from the implant-abutment connection. Instead, it uses a precision-milled 1.5° locking taper. When the abutment is seated, this creates a tight friction-fit often described as a "cold weld." This powerful mechanical lock provides stability and is highly resistant to the rotational forces that can cause screw loosening in conventional systems.
Furthermore, this connection forms a bacterial seal, which helps protect the crestal bone from microbial leakage—a key factor in maintaining long-term peri-implant tissue health.
Are Short Implants as Reliable as Longer Implants?
Yes, extensive clinical data demonstrates that Bicon SHORT® Implants have survival rates comparable to, and in some cases exceeding, those of longer implants placed in grafted bone. Their success is a function of design, not length.
Two features enable this high reliability:
- The plateau design: This geometry significantly increases the functional surface area available for osseointegration.
- The locking taper: This connection ensures that occlusal forces are distributed favorably along the implant body rather than being concentrated at the crestal bone.
This combination makes them a predictable and less invasive option for patients with limited bone height, often eliminating the need for complex augmentation procedures.
What Is the Learning Curve for a Clinician New to Bicon?
The primary adjustment is surgical. Clinicians must become proficient with the slow-speed osteotomy preparation and the tap-in, press-fit placement technique, which provides different tactile feedback than high-torque insertion.
On the restorative side, the main shift involves understanding the Integrated Abutment Crown (IAC) and mastering the 360° universal abutment positioning. While this offers significant flexibility, it represents a new workflow.
Although it is a departure from conventional systems, most clinicians find the workflow to be logical and efficient once they have completed initial training, as it is designed to simplify clinically challenging situations.
Alfa Gate offers a comprehensive portfolio of implant systems designed to meet the diverse needs of modern dental practices. To learn more about our innovative solutions, explore our advanced Bioactive implant systems or get in touch to discuss how our products can enhance your clinical offerings. For partnership opportunities, learn how to become a distributor for Alfa Gate.







