A Clinician's Guide to Using Lasers in Dental Practice
Dental lasers, once a futuristic concept, are now an indispensable tool in modern clinical practice. This technology leverages highly focused light to perform precise, minimally invasive treatments on both soft and hard tissues. The clinical advantages are significant: reduced bleeding, minimal patient discomfort, and accelerated healing times compared to traditional scalpel and suture techniques.
The Modern Role of Lasers in Dentistry

Integrating laser technology is a fundamental shift toward enhancing precision and improving patient outcomes. What was once a niche instrument is now a standard for daily procedures, from routine soft-tissue management to the complex demands of implantology.
This adoption is driven by tangible clinical benefits. For clinicians, lasers provide unparalleled control, enabling clean incisions with simultaneous haemostasis. This creates a clear, bloodless surgical field, improving visibility and procedural efficiency.
Elevating the Standard of Care
The advantages for patients are even more compelling. Because laser treatments are minimally invasive, patients often experience:
- Less need for anaesthesia in many procedures.
- Noticeably reduced post-operative pain and swelling.
- A faster, more comfortable healing process.
- A lower risk of bacterial infection due to the laser's sterilising properties.
This significant improvement in patient care is a powerful differentiator for any practice. In implant dentistry, for example, lasers are invaluable for sculpting soft tissue around abutments—like those in the Alfa Gate M+ Conical Connection system—to achieve optimal aesthetic results and support long-term osseointegration.
A Strategic Clinical Investment
Adopting laser technology is a strategic decision to future-proof a dental practice. This trend is evident in markets with advanced healthcare systems. Germany, for instance, holds the largest revenue share in the European dental lasers market, commanding approximately 29% of the market. This is a direct result of patient demand for treatments that promise less pain and faster recovery. For more data, you can discover key insights into the European dental market here.
For clinicians and distributors, understanding the practical applications and financial viability of this technology is crucial for staying competitive and delivering the highest standard of care.
How Different Dental Lasers Work
Understanding the mechanism of a dental laser does not require a background in physics. The effectiveness of a laser is determined by its wavelength and how that specific wavelength interacts with the target oral tissue.
Different biological tissues—from haemoglobin-rich soft tissue to hydroxyapatite-based hard tissue—absorb light at different rates.
A laser's specific wavelength is absorbed by designated molecules, known as chromophores. This precise absorption allows the laser to cut, vaporise, or coagulate with pinpoint accuracy, leaving adjacent tissues virtually untouched. This core principle differentiates laser types and dictates their clinical applications. Therefore, selecting the appropriate laser is a clinical decision based on the tissue being treated.
The Soft-Tissue Specialists
Certain lasers are specifically designed for soft-tissue applications due to their wavelengths' high absorption by pigments and haemoglobin.
- Diode Lasers: These are the workhorses of many modern practices. With wavelengths typically in the 810-980 nm range, they are strongly attracted to melanin and haemoglobin. This makes them ideal for procedures like gingivectomies and frenectomies, where their ability to coagulate blood vessels on contact provides immediate haemostasis.
- Nd:YAG Lasers: The Neodymium-doped Yttrium Aluminium Garnet (Nd:YAG) laser, with its 1064 nm wavelength, also targets pigment. It can penetrate deeper into tissue, making it an effective tool for bacterial reduction in periodontal pockets and treating certain vascular lesions.
Both Diode and Nd:YAG lasers create a clean, dry surgical field. The focused energy also seals nerve endings during incision, which often results in significantly less post-operative pain for the patient.
The Hard-Tissue Experts
Hard-tissue lasers operate on a different principle. Their energy is not absorbed by pigment but by water and hydroxyapatite—the primary components of enamel, dentin, and bone.
These lasers function by targeting water molecules within hard tissues. The intense energy causes this water to expand and vaporise in a process called photoablation. This allows for precise cutting of tooth structure and bone with minimal thermal damage to the surrounding area.
- Er:YAG Lasers: The Erbium-doped Yttrium Aluminium Garnet laser has a wavelength of 2940 nm, which closely matches the peak absorption of water. This makes it an incredibly efficient tool for cavity preparations, bone surgery, and implant site preparation.
- CO2 Lasers: While older 10,600 nm CO2 lasers were primarily soft-tissue instruments, newer 9,300 nm versions are also absorbed by hydroxyapatite. This evolution makes them remarkably versatile for both soft-tissue contouring and hard-tissue ablation.
The ability to work on bone and enamel without the vibration and heat of a mechanical drill is a significant advancement in patient comfort. For clinicians focused on achieving reliable osseointegration and predictable outcomes, understanding these tools is essential. For further reading, explore our guide on Strategies for Successful Bone Regeneration.
A Practical Comparison of Dental Laser Types
This table provides a side-by-side comparison to help match the right technology to the right clinical task.
| Laser Type | Wavelength | Primary Target Tissue | Key Clinical Applications |
|---|---|---|---|
| Diode | 810–980 nm | Haemoglobin & Melanin | Gingivectomy, Haemostasis, Bacterial Reduction |
| Nd:YAG | 1064 nm | Haemoglobin & Melanin | Periodontal Therapy, Soft-Tissue Surgery |
| Er:YAG | 2940 nm | Water & Hydroxyapatite | Cavity Preparation, Bone Surgery, Implant Site Prep |
| CO2 | 9,300–10,600 nm | Water & Hydroxyapatite | Soft-Tissue Contouring, Hard-Tissue Ablation |
Ultimately, choosing a laser is a strategic decision that aligns the best technology with your clinical objectives. To explore which systems fit your practice or distribution network, we invite you to become a distributor and begin the conversation.
A Better Way to Handle Soft-Tissue and Periodontal Work
The precision and haemostatic properties of dental lasers offer significant advantages over traditional instruments in soft-tissue and periodontal cases. A laser in dental procedures seals small blood vessels as it incises, ensuring a clear, dry surgical field. This enhances accuracy whether sculpting gingival margins or performing a frenectomy.
Getting a Handle on Common Soft-Tissue Procedures
For routine soft-tissue surgeries, the benefits are immediate for both the clinician and the patient. A diode or CO2 laser vaporises tissue with minimal collateral thermal damage, leading to less inflammation and a more comfortable recovery.
For example, in a gingivectomy, a laser allows for layer-by-layer tissue removal while simultaneously controlling bleeding. Sutures are often unnecessary, healing is faster, and the final aesthetic contours are more predictable. The same applies to frenectomies, where the laser's clean incision minimises scarring and promotes faster functional recovery.
This infographic illustrates how different laser wavelengths interact with key oral tissue components.
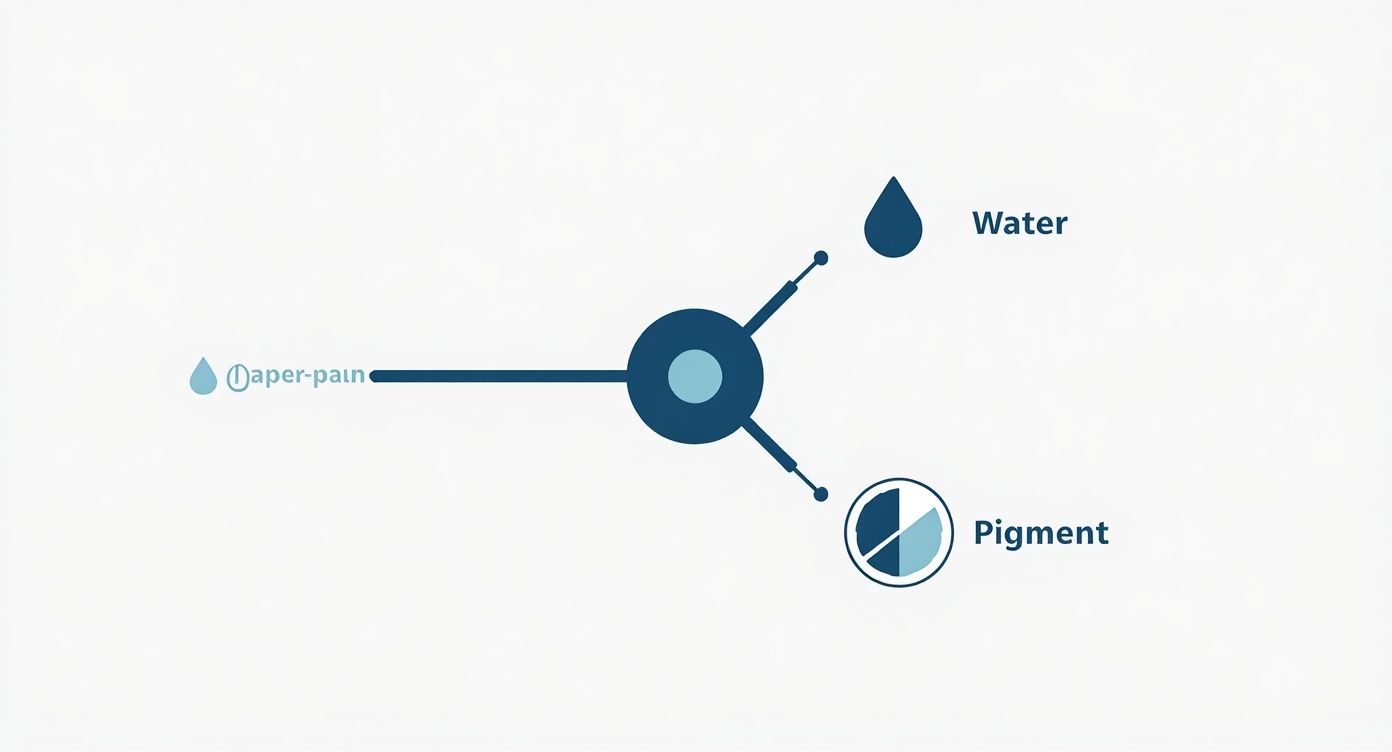
As shown, some lasers target water (ideal for hard tissues), while others are absorbed by pigment, making them effective for soft-tissue management.
Stepping Up Your Periodontal Therapy
In periodontics, a laser's bactericidal properties are a key advantage. When a laser fibre is guided into a periodontal pocket, its energy can eliminate a significant portion of the bacterial load, including pathogens resistant to conventional methods.
This technique, known as laser-assisted bacterial reduction (LBR), complements traditional scaling and root planing. The laser's energy specifically targets pigmented bacteria like Porphyromonas gingivalis without harming healthy tissue. This decontaminates the pocket and stimulates the gingiva's natural healing response.
A practical example is the LANAP protocol (Laser-Assisted New Attachment Procedure), which aims not only to eliminate bacteria but also to potentially regenerate the periodontal ligament and bone. It offers a less invasive alternative to traditional flap surgery.
For implant placement, maintaining healthy peri-implant soft tissue is critical. The precise incision made by a laser during tissue management is comparable to that of highly specialised instruments. For similar predictability during implant exposure, tools like the Alfa Gate Tissue Punch can achieve a perfect circular cut.
The Practical Upside in Your Daily Practice
Integrating a laser for soft-tissue and periodontal work offers tangible patient benefits.
- Less Discomfort: Lasers seal nerve endings as they work, resulting in significantly less post-operative pain.
- Quicker Healing: Minimally invasive laser surgery leads to less bleeding and inflammation, promoting faster patient recovery.
- Improved Patient Experience: The absence of a blade and reduced need for anaesthesia can lower patient anxiety, improving case acceptance.
Using a laser is about refining clinical technique to deliver more predictable, efficient, and comfortable patient outcomes.
Enhancing Dental Implant Procedures with Lasers

While beneficial in soft-tissue care, the true power of a laser in dental implantology is evident throughout the entire workflow. From site preparation to final aesthetic contouring, lasers provide a degree of precision that complements high-quality implant systems, ensuring predictable and stable results.
During the healing phase, a laser can be used for implant exposure. It precisely vaporises the gingival tissue covering the implant, creating a bloodless field that simplifies the placement of the healing abutment.
Precision Soft-Tissue Management Around Implants
Aesthetic success in implant dentistry depends heavily on soft-tissue management. A laser acts as a precision instrument, allowing for meticulous sculpting of the gingiva to create natural emergence profiles.
A common application is troughing, where a small channel is created around the implant abutment before taking an impression. This technique displaces the gingiva, ensuring the impression material captures the entire margin accurately for a perfectly fitting final crown.
A diode laser offers a significant advantage over retraction cord. Instead of mechanically displacing tissue, the laser gently removes it while achieving haemostasis. This creates a dry, clear field essential for accurate digital scans or conventional impressions, leading to restorations that blend seamlessly.
Treating and Preventing Peri-implantitis
A critical role for lasers in implantology is managing peri-implant diseases. Peri-implantitis is an inflammatory condition that can cause bone loss and implant failure. The primary challenge is decontaminating the implant surface without altering its micro-topography.
Specific laser wavelengths, particularly from Er:YAG lasers, are ideal for this task. Their energy is absorbed by water, allowing them to ablate bacterial biofilm and calculus from the implant surface with minimal heat transfer. This laser-assisted detoxification can halt disease progression and create an environment conducive to osseointegration.
- Surface Decontamination: The laser can access implant threads where conventional instruments cannot, removing bacteria without damaging the implant surface.
- Reduced Inflammation: Eliminating the bacterial load helps reduce gingival inflammation and pocket depths around the implant.
- Support for Regeneration: A decontaminated surface is an ideal foundation for bone grafting procedures to rebuild lost bone.
For a comprehensive overview of surgical protocols, refer to our dental implant surgery guide for dentists.
Creating the Perfect Aesthetic Outcome
Beyond troughing, lasers provide pinpoint control over the final gingival architecture. After seating the final restoration, clinicians can correct minor asymmetries or remove excess tissue with precision.
This detailed soft-tissue sculpting helps create ideal gingival contours and papillae, beautifully framing the restoration. The result is an aesthetic outcome that is nearly indistinguishable from a natural tooth, elevating a good result to an exceptional one.
Integrating Lasers Safely and Efficiently
Integrating a laser into clinical practice requires a robust framework for safety and workflow efficiency. This is a fundamental responsibility to protect patients, staff, and clinicians.
The process begins with establishing a controlled environment. Wavelength-specific protective eyewear is mandatory for everyone in the operatory whenever a laser is active. High-volume evacuation must be used to manage the laser plume, and clear signage should control access to the room.
Establishing a Culture of Safety
A designated Laser Safety Officer (LSO) is central to a successful laser program. This individual, typically a dentist or trained team member, champions laser safety by overseeing equipment checks and ensuring compliance with all standards.
The LSO's key responsibilities include:
- Protocol Development: Creating and maintaining clear safety protocols for all laser procedures.
- Team Training: Ensuring every team member receives certified training relevant to their role.
- Equipment Maintenance: Overseeing regular maintenance and calibration of all laser devices.
- Record Keeping: Maintaining meticulous logs of laser use, safety audits, and staff training as required by regulations.
The Critical Role of Certified Training
Competency and safety in laser dentistry are achieved only through comprehensive, certified training for the entire clinical team. This education must cover laser physics, tissue interaction, and procedure-specific protocols. A well-trained team not only operates the device safely but also understands the clinical nuances required for optimal patient outcomes.
Proper training empowers clinicians to select the correct parameters—power, pulse duration, and frequency—for each procedure. This knowledge is what differentiates proficient laser dentistry from simple technology use and directly impacts treatment safety and efficacy.
Patient demand for minimally invasive procedures is growing. The Europe medical laser systems market was valued at $1.38 billion and is projected to grow at a CAGR of 14.7% through 2031. Germany is a significant contributor to this growth, where lasers are used to reduce operative risks and accelerate patient recovery. You can learn more about these market findings on medical laser systems.
Seamless Workflow Integration
Once safety protocols are established, the next step is integrating the laser into the daily workflow. A laser should be a complementary tool that enhances existing digital technologies like intraoral scanners and milling units.
For example, using a laser for troughing before a digital scan produces exceptionally clear margins, a concept detailed in our guide to understanding CAD/CAM dental technology. This synergy between technologies helps maximise the return on investment and elevate the standard of care.
Is a Dental Laser a Smart Investment? Let's Run the Numbers.
When considering a dental laser, a Return on Investment (ROI) analysis provides a clearer picture than the initial purchase price alone. A comprehensive assessment should evaluate how the technology generates new revenue, improves practice efficiency, and enhances patient care.
This analysis requires accounting for both capital expenditures and operational costs.
Breaking Down the Costs
A realistic ROI forecast includes several key figures:
- The Initial Outlay: The capital expenditure for the laser unit.
- Upkeep and Servicing: Annual service contracts and potential repair costs.
- Consumables: Disposable items such as laser tips.
- Team Training: The cost of certified education to ensure safe and effective operation.
These represent the "investment" side of the equation. The "return" is often where clinicians see the greatest value.
Unlocking New Ways to Generate Revenue
The financial strength of a dental laser lies in its ability to expand the scope of procedures offered. This allows practices to keep more complex cases in-house and attract patients seeking modern, minimally invasive treatments.
New services can include:
- Cosmetic Soft-Tissue Work: Gingivectomies and crown lengthening for aesthetic cases are high-value, private-pay treatments.
- Next-Level Periodontal Therapy: Laser-assisted therapies offer a premium alternative to traditional surgery.
- Peri-Implantitis Management: Treating and saving failing implants is a highly specialised service that improves long-term patient oral health.
These services align with growing patient demand. The German dental devices market is projected to reach US$1.82 billion, driven by cosmetic and preventive treatments. This trend supports investment in advanced laser technology. You can see more data on the German dental device market for further insights.
A Practical Checklist for Making the Right Choice
A smart purchasing decision extends beyond financials. The right laser is a long-term clinical asset, and the quality of support is as important as the technology itself.
When evaluating options, consider the manufacturer's reliability and commitment to clinical success. An inexpensive device can become costly if it requires frequent repairs or if the training is inadequate.
Before making a commitment, ensure you have clear answers to these questions:
- How comprehensive is the manufacturer's training and ongoing clinical support?
- What is the company's reputation for building reliable, durable devices?
- Is service and support readily available in your region?
Investing in a dental laser is a strategic move to future-proof your practice. It expands your clinical capabilities, works in synergy with proven solutions like our Alfa Gate Implant Systems, and reinforces your reputation for patient-centred care.
Your Questions About Dental Lasers, Answered
When considering laser technology, several common questions arise. Clear answers can help demystify this technology and illustrate its practical clinical applications.
What’s the Real Advantage of a Laser Over a Scalpel?
The primary advantage is haemostasis. A laser's energy coagulates blood vessels on contact, creating a nearly bloodless surgical field.
This provides a clear view of the surgical site, reduces post-operative swelling, and often eliminates the need for sutures. The result is a faster, more comfortable healing process, which is a significant benefit in aesthetic and implant dentistry.
Can I Get One Laser That Does It All—Hard and Soft Tissue?
No, a single laser cannot optimally treat both hard and soft tissues. The appropriate laser is determined by its wavelength. Diode and Nd:YAG lasers are absorbed by pigment, making them ideal for soft tissue.
Conversely, lasers like the Er:YAG are absorbed by water and hydroxyapatite, enabling them to cut enamel and bone with minimal thermal damage.
Selecting a laser is like choosing the right tool for a specific task. One device cannot be optimised for two distinct tissue types, which is why practices typically choose a laser based on their most frequently performed procedures.
What's the Learning Curve Like for a Dental Laser?
The learning curve depends on the intended application. Basic soft-tissue procedures with a diode laser are relatively straightforward to master.
However, advanced applications like periodontal therapy or bone cutting require comprehensive, certified hands-on training. Reputable manufacturers provide robust educational support to ensure clinical competency and safety from the outset.
Mastering the use of a laser in dental practice requires understanding its capabilities and limitations. When this knowledge is combined with high-quality systems, such as versatile Alfa Gate Prosthetic components, laser technology introduces a new level of precision to all aspects of dentistry.
At Alfa Gate, our mission is to provide clinicians with the advanced systems and expertise needed to deliver exceptional care. To learn more about our innovative implant solutions or to explore partnership opportunities, we invite you to contact our team.







