A Clinician's Guide to All-on-4 Dental Implants
The All-on-4 treatment concept represents a significant advancement in full-arch rehabilitation for edentulous patients. This protocol facilitates the delivery of a fixed, full-arch prosthesis, often on the day of surgery. Its primary clinical advantage lies in the use of tilted posterior implants to engage denser anterior bone, thereby avoiding critical anatomical structures and frequently eliminating the need for complex bone grafting procedures. This approach results in a less invasive, more time-efficient, and highly predictable clinical outcome.
The Clinical Rationale Behind the All-on-4 Concept
Historically, full-arch reconstruction in patients with significant posterior bone atrophy presented a formidable challenge. Conventional protocols often required six to eight vertically placed implants, a strategy that necessitated extensive bone augmentation procedures like bilateral sinus lifts or nerve repositioning to create adequate bone volume. These ancillary surgeries increased treatment time, cost, and patient morbidity, often acting as a barrier to case acceptance.
The All-on-4 concept was developed to address these limitations directly. It is founded on the biomechanical principle of maximizing the use of available native bone in the anterior region, where bone quality and volume are typically superior and less prone to resorption.

Maximising Available Anatomy
The strategic tilting of the two posterior implants, up to a 45-degree angle, is the cornerstone of this technique. This angulation achieves several critical objectives simultaneously:
- Avoidance of Vital Structures: It allows the clinician to circumvent the maxillary sinus in the upper arch and the mental foramen in the lower arch, mitigating surgical risks.
- Engagement of Denser Bone: Implants are anchored in the higher-quality anterior bone, which is essential for achieving the high primary stability required for immediate loading protocols.
- Increased Anteroposterior Spread: Tilting the implants creates a wider, more stable prosthetic base. This results in a more favorable biomechanical distribution of occlusal forces and reduces stress on the final restoration.
This innovative use of angulation transforms a potentially complex, graft-dependent case into a streamlined, graftless procedure. A treatment timeline that might have extended beyond a year can be condensed to a few months. Clinical data supports the efficacy of this approach; a 2022 retrospective study reported a cumulative implant survival rate of 89.7% over an average of 6.5 years. You can read the full findings about All-on-4 success rates for a deeper analysis.
Engineered for Predictable Outcomes
The success of the All-on-4 technique is contingent upon using implant systems engineered for high primary stability. Alfa Gate’s advanced systems, such as the DFI implant, feature designs with aggressive thread patterns and tapered bodies that excel in immediate load scenarios. These characteristics ensure robust initial fixation, which is the non-negotiable foundation for predictable osseointegration and a successful long-term prosthesis.
Mastering Patient Selection and Diagnostics
Successful implementation of the All-on-4 protocol begins with meticulous patient selection and a comprehensive diagnostic workup. A robust evaluation process is fundamental not only for clinical success but also for establishing realistic patient expectations. The process initiates with a thorough review of the patient's medical and dental history, followed by a clinical examination of soft tissues, remaining dentition, and occlusal relationships.
Cone Beam Computed Tomography (CBCT) is an indispensable diagnostic tool for this protocol. A CBCT scan provides a detailed three-dimensional assessment of the jaw, enabling precise measurement of bone volume and density, particularly in the critical anterior regions where implants will be anchored.

Differentiating Ideal Candidates from Complex Cases
The ideal candidate for an All-on-4 procedure is typically a patient with a fully edentulous arch or one with a terminal dentition. The primary prerequisite is sufficient bone quality and quantity in the anterior maxilla or mandible. Good general health and a commitment to maintaining excellent long-term oral hygiene are also essential.
Conversely, certain conditions may require careful consideration or contraindicate the procedure entirely.
A meticulous diagnostic phase, built around a thorough CBCT analysis, is non-negotiable. It transforms a treatment plan from a conceptual outline into a precise surgical roadmap, directly impacting implant stability and the final prosthetic outcome.
Understanding Key Contraindications
Early identification of potential risk factors is a cornerstone of effective clinical risk management. While few conditions are absolute contraindications, several require interdisciplinary collaboration or modifications to the standard treatment plan.
Absolute Contraindications:
- Uncontrolled Systemic Diseases: Conditions such as unmanaged diabetes or a recent myocardial infarction significantly increase surgical risks and can impair osseointegration.
- Intravenous Bisphosphonate Therapy: These patients are at an elevated risk for medication-related osteonecrosis of the jaw (MRONJ).
- Active Chemotherapy or Radiation Therapy: These treatments can severely compromise the body's healing capacity and bone quality.
Relative Contraindications:
- Heavy Smoking: Smoking is a significant risk factor for implant failure and peri-implantitis, necessitating a detailed discussion with the patient about risks and cessation.
- Severe Parafunctional Habits: Unmanaged bruxism can generate excessive forces on the immediate prosthesis, threatening the stability of newly placed implants.
- Inadequate Interarch Space: Insufficient vertical dimension can complicate the fabrication of the final prosthesis and may require a preliminary alveoloplasty.
- Poor Oral Hygiene: A patient's inability or unwillingness to maintain proper oral hygiene is a strong predictor of long-term complications. You can learn more about tackling these issues in our article on peri-implantitis experiences and solutions.
Successful patient selection involves balancing patient desires with clinical realities. A firm understanding of these diagnostic principles provides the confidence to proceed with treatment, ensuring more predictable and durable outcomes for every All-on-4 case.
Biomechanical Principles for Long-Term Success
The long-term success of any All-on-4 case is fundamentally rooted in sound biomechanical principles. The technique's hallmark—the strategic tilting of posterior implants—is an application of biomechanical engineering designed to optimize force distribution. By angling these implants, clinicians can dramatically increase the anteroposterior (AP) spread, which is the distance between the most anterior and most posterior implants.
A wider AP spread creates a more stable foundation for the prosthesis, distributing occlusal forces more evenly across the entire arch. This reduces stress on individual implants and, critically, minimizes distal cantilevers, a known source of mechanical complications.
Implant Positioning: Traditional vs. All-on-4
This table contrasts the All-on-4 concept with traditional approaches, highlighting its biomechanical advantages in atrophic jaws.
| Factor | Traditional Full-Arch (6-8 Implants) | All-on-4 Protocol |
|---|---|---|
| Number of Implants | Typically 6-8 implants, placed vertically. | 4 implants (2 anterior, 2 tilted posterior). |
| AP Spread | Limited by posterior bone availability. Often requires grafting. | Maximised by tilting posterior implants, avoiding sinuses/nerves. |
| Cantilever Length | Often necessary to restore full molar occlusion, increasing stress. | Dramatically reduced or eliminated, lowering mechanical risk. |
| Surgical Invasiveness | High. Frequently requires extensive bone grafting procedures. | Minimally invasive; designed to use existing native bone. |
| Load Distribution | Spread across more implants, but placement can be compromised. | Strategically distributed across a wider, more stable base. |
The All-on-4 protocol is not merely about reducing the number of implants; it represents a more intelligent strategy for managing biomechanical forces for immediate function.
Primary Stability: The Non-Negotiable Foundation
For immediate loading protocols, achieving high primary stability is non-negotiable. This initial mechanical engagement of the implant within the bone is the bedrock for successful osseointegration. The clinical benchmark for a predictable outcome in an All-on-4 case is an insertion torque of at least 35 Ncm.
Failure to achieve this threshold risks micromovement at the bone-implant interface, which can lead to fibrous encapsulation rather than osseointegration. The choice of implant system is therefore paramount. The German dental implants market, valued at USD 437.6 million in 2024, continues to grow, driven by innovations that support advanced treatments like All-on-4. You can discover more insights about the German dental implant market for industry trends.
The Right Implant Design for the Job
Not all implant designs are suited for the demands of the All-on-4 technique. To achieve immediate, unwavering stability, specific design features are required.
- Aggressive Thread Design: Deep, sharp, self-tapping threads enable the implant to actively engage and compress bone during placement, ensuring a powerful mechanical lock.
- Tapered Body: A conical or tapered morphology provides a wedge effect, compressing the surrounding bone to enhance initial grip, particularly in softer D3 or D4 bone.
- Robust Conical Connection: A deep conical implant-abutment connection creates a tight seal that minimizes micromovement and protects the crestal bone from bacterial ingress and mechanical stress.
The clinical efficacy of the All-on-4 concept is realized when a wide AP spread is combined with high primary stability. Implant tilting solves the biomechanical challenge, while a well-designed implant provides the mechanical fixation required for immediate function.
The Alfa Gate DFI implant exemplifies a system engineered for this purpose. Its tapered body, double-lead threads, and proven conical connection are designed to deliver the high primary stability that immediate loading protocols demand.
This focus on biomechanics elevates the All-on-4 from a surgical technique to a predictable, life-changing solution. To learn how to integrate these advanced solutions into your practice, we invite you to become a distributor.
Integrating the Digital Workflow into Clinical Practice
The predictability of the All-on-4 approach is significantly enhanced by modern digital workflows. By replacing traditional analog methods with a fully digital process, clinicians can navigate from diagnosis to final restoration with unprecedented precision. This systematic approach reduces clinical variables, shortens chair time, and improves patient outcomes.
The workflow begins by merging data from an intraoral scanner, which captures a highly accurate digital impression of the patient's soft tissues, with data from a Cone Beam Computed Tomography (CBCT) scan. This fusion creates a comprehensive 3D virtual model of the patient's anatomy.
Meticulous Virtual Implant Planning
Within the planning software, implants can be placed virtually with sub-millimeter accuracy. Clinicians can adjust position, angulation, and depth to optimize engagement in high-quality bone while avoiding vital structures.
This virtual planning serves as a surgical rehearsal, offering key advantages:
- Optimal Implant Positioning: Different placements can be simulated to achieve the ideal anteroposterior spread, ensuring robust biomechanical support for the prosthesis.
- Prosthetic-Driven Planning: The implant positions are determined with the final restoration in mind, ensuring a functional and aesthetic outcome.
- Risk Mitigation: Critical anatomical structures, such as the inferior alveolar nerve and maxillary sinus, are clearly visualized, allowing for safe surgical planning.
The Alfa Guide System for Guided Surgery
The culmination of digital planning is the fabrication of a patient-specific surgical guide. The Alfa Guide system translates the virtual plan into a physical template that precisely directs the drills and implant placement. This eliminates the guesswork of freehand surgery and ensures that each implant is placed exactly as planned.
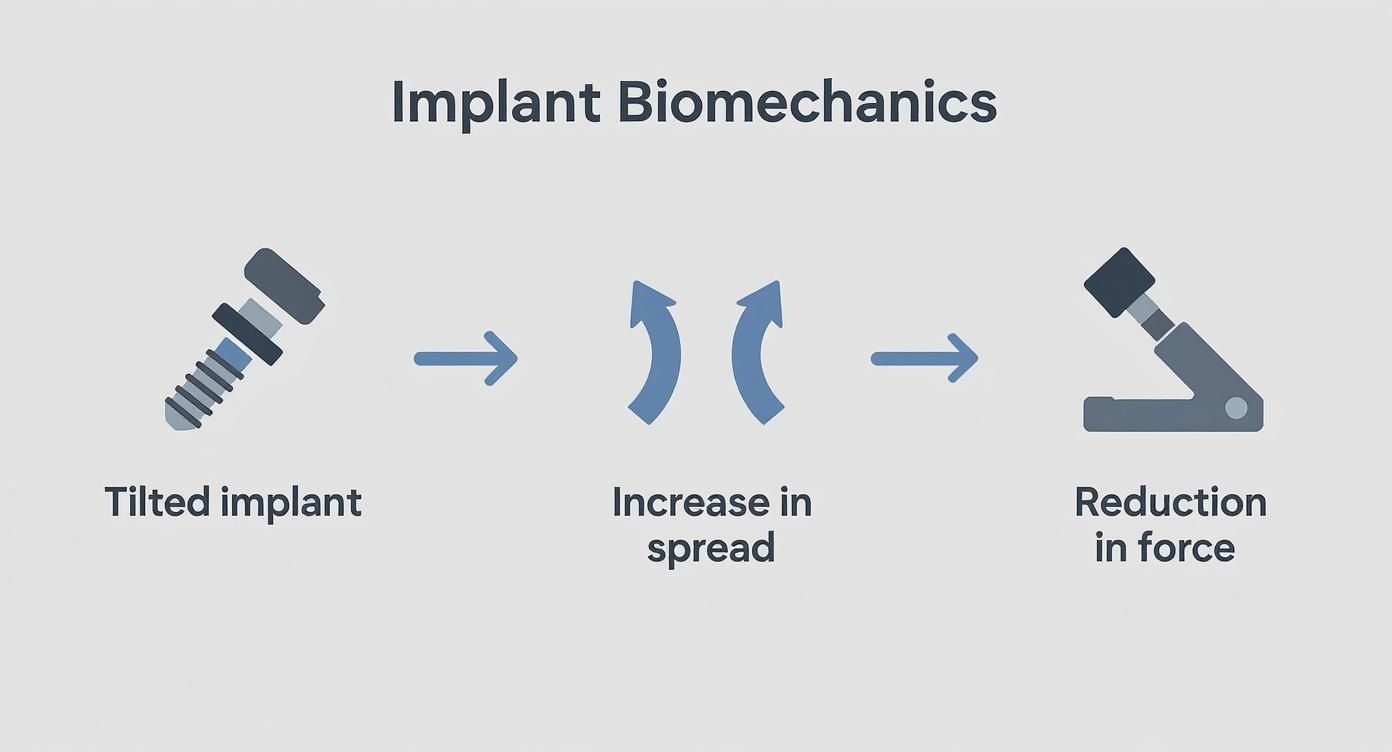
The infographic illustrates the core biomechanical principle optimized during digital planning: tilting posterior implants to widen the prosthetic foundation.
Guided surgery is the essential bridge between the digital plan and the clinical reality. It ensures the biomechanical advantages mapped out on the screen are perfectly reproduced in the patient's mouth, leading to safer, more predictable outcomes.
The benefits of a guided system like Alfa Guide include reduced surgical times and less invasive procedures, often allowing for flapless surgery. This translates to less post-operative discomfort and faster healing for the patient.
CAD/CAM Fabrication of Prosthetics
The digital workflow extends into the restorative phase. Both the provisional and definitive prostheses are designed in CAD software using the digital data. These designs are then sent to a milling unit or 3D printer for CAM fabrication.
CAD/CAM-fabricated prosthetics, whether milled from PMMA or zirconia, exhibit a superior passive fit compared to those made with traditional methods. This precision is critical, as it minimizes stress on the implants and framework, contributing to the long-term health of the supporting bone and the success of the restoration. By embracing a complete digital workflow, clinicians can deliver All-on-4 treatments with greater confidence, efficiency, and a higher standard of care.
Prosthetic Component Selection and Restorative Protocols
The restorative phase of an All-on-4 treatment is where surgical planning culminates in a functional and aesthetic outcome for the patient. Success hinges on the appropriate selection and use of prosthetic components. These components are precision-engineered to solve complex biomechanical and aesthetic challenges.
The key components in the All-on-4 protocol are multi-unit abutments (MUAs). These abutments provide the necessary flexibility to manage varying implant angulations. By combining straight and angled MUAs, clinicians can correct for the tilted posterior implants and the axial anterior ones to create a single, level restorative platform. This parallelism is essential for achieving a passive fit, where the final prosthesis seats on the abutments without any stress or tension.
A passive fit is the cornerstone of long-term prosthetic success. A non-passive framework induces stress that can lead to mechanical complications, such as screw loosening or fracture, and can transfer damaging forces to the implants, potentially jeopardizing osseointegration.
Material Choices for Provisional and Definitive Prostheses
The restorative process involves two distinct phases, each requiring a prosthesis made from specific materials.
1. The Immediate Provisional Prosthesis
Following surgery, an immediate provisional prosthesis is delivered. This is typically fabricated from a high-impact acrylic (PMMA) reinforced with an internal metal or carbon fiber bar. Its functions are to provide immediate aesthetics and function, protect the healing tissues, and serve as a prototype for the final restoration. The slight flexibility of the acrylic material can help absorb occlusal forces while the implants are integrating.
2. The Definitive Prosthesis
After a healing period of several months, the definitive prosthesis is fabricated. Modern material options include:
- Full Monolithic Zirconia: This material offers exceptional strength, durability, and aesthetics. Zirconia is highly biocompatible and resistant to plaque accumulation, promoting peri-implant tissue health.
- Titanium-Hybrid Prosthesis: This design combines a precision-milled titanium bar for strength and a passive fit, with either acrylic denture teeth and gingiva or individual zirconia crowns cemented to the framework. This approach offers excellent aesthetics and facilitates easier repairs if needed.
Occlusion and Passive Fit Verification
Establishing the correct vertical dimension of occlusion (VDO) is crucial for patient comfort and function. The provisional prosthesis serves as a "test drive" to fine-tune the VDO, allowing the patient to adapt and provide feedback before the definitive prosthesis is designed. The goal is to create a comfortable occlusal relationship with adequate space for all prosthetic components, without placing strain on the patient's masticatory muscles.
Achieving a tension-free, passive fit requires precision at every step. One highly effective method is the use of a verification jig. This is a rigid framework that connects the implant analogs on the master cast, allowing the clinician to confirm the accuracy of the model before fabricating the expensive final framework. This step helps prevent costly errors and ensures the final prosthesis seats perfectly without stress.
For a deeper technical review, read our guide on the clinical applications of Multi-Unit Abutments.
Proactive Complication Management and Maintenance Strategies
While successful placement of an All-on-4 restoration is a significant clinical achievement, long-term success is determined by its performance over time. This requires a proactive maintenance strategy designed to safeguard both the biological health of peri-implant tissues and the mechanical integrity of the prosthesis.
Openly discussing potential complications with patients builds trust and enlists them as active partners in their long-term care. These issues generally fall into two categories: biological and mechanical, each requiring distinct prevention and management strategies.
Identifying and Managing Biological Complications
The primary biological threat to any implant-supported restoration is peri-implant disease. The absence of a periodontal ligament makes implants more susceptible to inflammatory processes.
Peri-mucositis, a reversible inflammation of the soft tissues, is the initial stage. If left unaddressed, it can progress to peri-implantitis, an irreversible condition characterized by progressive bone loss that can lead to implant failure.
Establishing a rigorous, patient-specific recall programme is the cornerstone of long-term implant survival. This protocol should be initiated immediately following the placement of the definitive prosthesis.
A structured maintenance plan is non-negotiable for mitigating these risks. To learn more, read our detailed guide on peri-implantitis experiences and solutions.
Preventing and Addressing Mechanical Failures
While less common with precise planning and high-quality components, mechanical issues can occur. These typically involve the prosthetic components rather than the implants.
Common mechanical issues include:
- Screw Loosening or Fracture: Often the first indicator of a non-passive fit or excessive occlusal forces.
- Prosthesis Fracture: While rare with monolithic zirconia, acrylic or hybrid restorations may chip or fracture, especially in patients with parafunctional habits.
- Wear of Prosthetic Materials: Occlusal surfaces will exhibit wear over years of function, which may require periodic adjustments or eventual replacement.
Regular professional evaluation is key to identifying these issues before they escalate.
Establishing a Rigorous Recall Programme
A successful maintenance routine is a collaborative effort between the clinical team and the patient. Professional care is essential, but it must be complemented by the patient's commitment to daily home care.
A professional recall appointment should include:
- Clinical Evaluation: Thorough inspection of soft tissues for signs of inflammation, bleeding on probing, and probing depths.
- Radiographic Assessment: Periodic radiographs (typically annually) to monitor crestal bone levels and confirm osseointegration.
- Prosthesis and Abutment Check: Removal of the prosthesis for comprehensive cleaning of all components and inspection for wear or damage. Prosthetic screws should be replaced as recommended.
- Professional Cleaning: Debridement of implant surfaces and the prosthesis using implant-safe instruments, such as titanium or carbon fiber scalers.
In Germany, the All-on-4 procedure starts at approximately €7,000, offering significant value. A diligent maintenance routine is the best way to protect this investment. You can discover more insights about the cost of All-on-4 implants in different countries to provide patients with a broader perspective.
For practices looking to provide these advanced solutions, we invite you to become a distributor and partner with a company committed to clinical excellence.
Frequently Asked Clinical Questions
Even with established protocols like the All-on-4 concept, clinical questions arise. This section addresses common queries to enhance clinical decision-making.
When Should All-on-4 Be Chosen Over a Traditional Approach?
The primary indication for the All-on-4 concept is moderate to severe bone resorption in the posterior regions. If placing vertical implants would necessitate major grafting procedures, such as a sinus lift, the All-on-4 protocol should be considered.
The strategic tilting of posterior implants allows for engagement of denser anterior bone, thereby avoiding more invasive and costly augmentation procedures. This makes it a more efficient and less morbid option for patients with compromised bone volume.
How Does Implant Surface Impact Immediate Loading Success?
In an immediate loading protocol, the implant surface is an active biological component. Advanced surfaces, such as Alfa Gate’s bioactive hydrophilic surface, are engineered to attract blood and osteogenic cells to the implant.
This accelerated biological response is critical for achieving rapid osseointegration, especially when high primary stability must be maintained under immediate functional load. It provides the biological support needed to counteract the risks of micromovement. To this end, consider systems like the purpose-built Alfa Gate DFI implant.
For immediate loading, a hydrophilic surface acts as a clinical safeguard. It accelerates biological stability, which can be the determining factor between predictable osseointegration and failure.
What Are Key Design Factors for the Final Prosthesis?
Three factors are critical for the long-term success of the definitive prosthesis: material selection, a passive framework fit, and a well-designed occlusal scheme.
The chosen material must withstand occlusal forces while remaining repairable. The framework must seat passively on the Multi-Unit Abutments to prevent stress on the implants. Finally, the occlusion must be designed to minimize lateral forces and distribute loads evenly across the arch.
For more specific clinical inquiries or to learn how Alfa Gate can support your practice's needs for full-arch implant cases, our expert team is available for consultation.
Contact Us to Discuss Your Clinical Needs







